

Dianna Lemus, Principal Agent
Big Changes Coming to Medicare in 2026-What You Need to Know
Get the scoop on upcoming Medicare changes, including rising prescription drug prices, Medigap premium hikes, Part B premium increases, and updates to extra benefit qualifications. Request your FREE Medicare Review, or keep scrolling for more info.

By submitting this form, you agree to be contacted by a licensed insurance agent from WeCare Insurance Solutions at the phone number and/or email address you provided. You may receive phone calls, text messages, or emails regarding Medicare plan options and related services. Consent is not a condition of purchase. Message and data rates may apply. You can opt out at any time by replying STOP.
Medicare Costs Are Changing in 2026 — Are You Ready?
The 2026 Medicare updates include higher premiums, new RX cost rules, and tighter eligibility for extra benefits. Don’t get caught by surprise — learn what this means for you.
Medicare Price Changes for 2026
From Part B Premiums, to RX Price Increases
Medicare Part B Premium is Going Up
Part B is the foundation of Medicare, covering doctor visits, outpatient care, preventive screenings, and much more. But like many health costs, premiums are on the rise.
Medicare Part B Coverage
Medicare Part B covers essential medical care like doctor visits, outpatient services, preventive screenings, lab work, and more. It’s what most people rely on for day-to-day healthcare needs outside of a hospital stay. Without Part B, you’d be responsible for paying these costs completely out-of-pocket.
2026 Part B Premiums on the Rise
In 2025, the standard Part B premium is $185 per month. Starting January 2026, that premium will rise to $206 per month. Historically, Part B increases at a rate of 5.5%; cost of living increases are typically much less than this. It is hard for some seniors to keep up with these unpredictable price increases. At WCHS Insurance, we help you find strategies to manage it.
Strategies to Help Manage Costs
If you qualify, state Medicaid programs may pay part or all of your Part B premium. Some Medicare Advantage giveback plans also refund a portion (or all) of your monthly Part B premium. In addition, certain plans include extra benefits — like help with groceries, utilities, or over-the-counter items — that can ease the burden of rising medical expenses. Working with a licensed agent helps ensure you’re exploring all available strategies. That's what we are here for!


2026 Medicare RX Prices
The standard Part D deductible and cost-sharing are going up — meaning you could pay more out of pocket before your plan begins covering your medications. Staying ahead of these changes now can help you avoid surprise expenses later.
RX Deductible on the Rise
In 2025, the maximum Part D deductible for a plan is $590. In 2026, it will increase to $605. This means you’ll need to spend more out of pocket before your plan starts sharing the cost of prescriptions. If you take multiple medications, this higher upfront cost can add up quickly. It's important to shop every year so that you know how much you can expect to pay out of pocket.
New Medicare Payment Structure
Starting in 2025, Medicare got rid of the "Donut Hole" and introduced a cap on out-of-pocket costs for prescriptions. This meant that plan members would pay no more than $2000 annually for prescription copays. In 2026, this is increasing to $2,100.
Strategies to Reduce RX Costs
Reviewing your plan each year is the best way to lower costs. Switching to preferred pharmacies, using mail order programs, or applying for Extra Help (Low-Income Subsidy) can dramatically cut your prescription spending. In addition, Medicare has a new Payment Plan option. It allows you to spread out the cost of medications over the year instead of paying a high amount up front. A licensed agent can help you compare plans and identify savings opportunities to fit your needs.
Medicare Supplement Plan Increases
Even though Medigap plans provide valuable coverage, premiums tend to rise as you age. Understanding why these increases happen—and what options you have—can help you keep your coverage affordable.
Why Medigap Prices Increase
Most Medigap plans use attained-age rating, meaning your premium increases as you get older. Insurance companies may also raise rates for inflation, rising healthcare costs, or to balance claims across the group. Over time, this can make even the most affordable plan feel expensive.
Exploring Alternative Options
Depending on your health and location, you may be able to switch to a different Medigap plan or even consider a Medicare Advantage plan. Comparing options can reveal savings opportunities without sacrificing coverage. It’s important to act during the right enrollment windows to avoid medical underwriting.
Strategies to Get Lower Premiums
Consider moving to a lower-cost Medigap plan (like switching from Plan G to a High-Deductible Plan G), or reviewing Medicare Advantage alternatives. If you are healthy enough, you may qualify for the EXACT same coverage with a different company. Talking to a licensed agent can help you find the balance between monthly cost and the coverage you rely on.

Medicare Advantage Extra Benefits Changes
Many Medicare Advantage plans offer monthly allowances for groceries and utilities. Starting in 2026, only those with qualifying chronic health conditions will be eligible for this benefit. It’s important to know what this means for you and how to prepare.
Who Will Qualify in 2026?
In 2025 and previous years, extras like the Grocery allowance and utility assistance have been available to those receiving Medicare + Medicaid (D-SNP plans). Beginning in 2026, these benefits may still be available on many plans, but Medicare requires that members have a chronic condition (such as diabetes, heart disease, or COPD) to qualify for the Healthy Food Benefit. This means the benefit will no longer be automatically included for all enrollees—it will be tied to health status.
Why the Change?
CMS wants to ensure that food and nutrition support goes to those with chronic illnesses who are most likely to benefit. While this creates more targeted support, it may leave some current members without access to the grocery allowance they’ve counted on. On the flip side, many people with chronic conditions will be able to qualify for more benefits than in previous years.

What to do if I no Longer Qualify?
Even if you don’t meet the chronic condition requirement, some plans may offer other supplemental benefits such as over-the-counter benefits, dental, or vision coverage. Reviewing your plan choices during enrollment is the best way to see if you can still access benefits that help offset everyday costs.
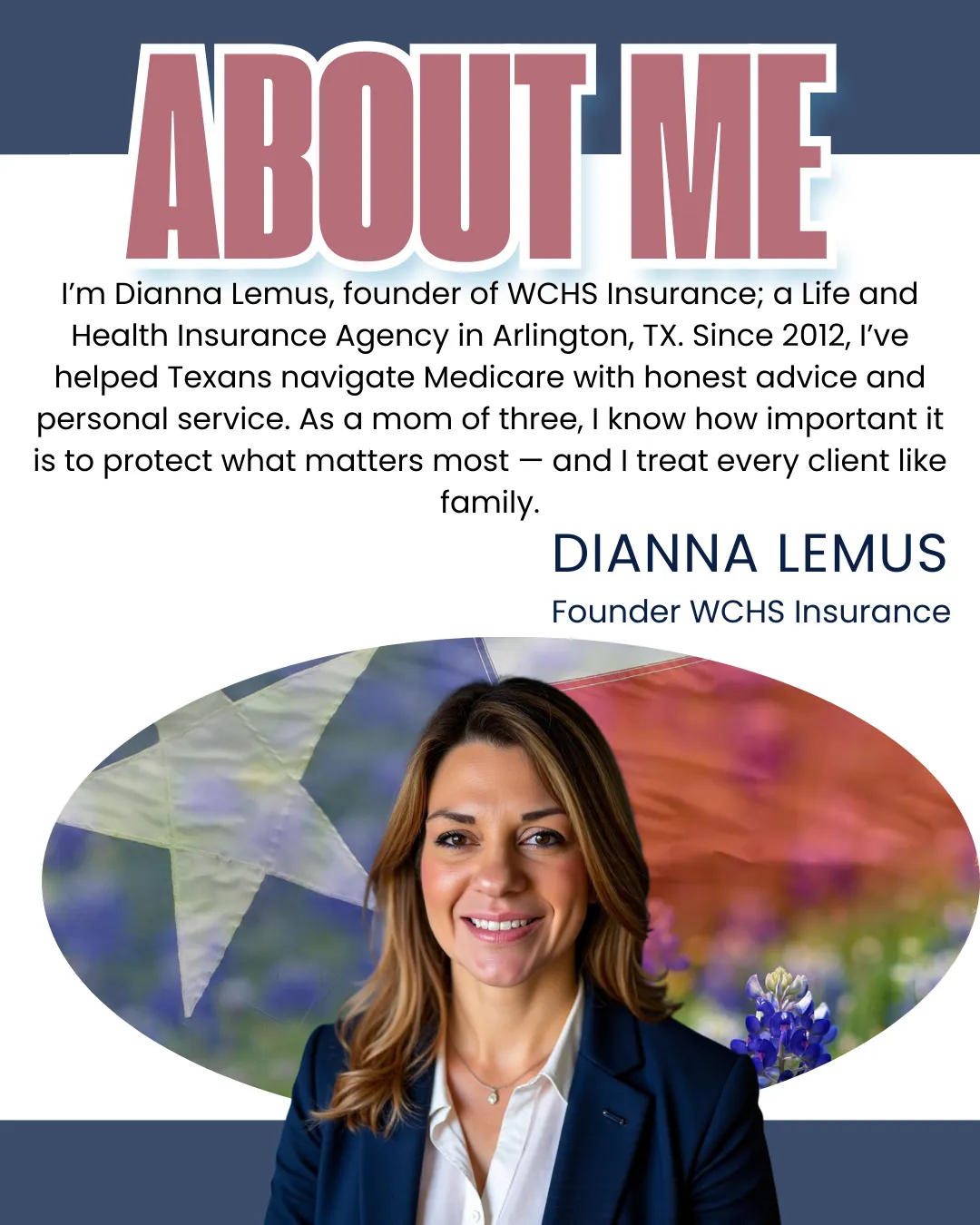
Why Texans Choose Us
Independent, Local Agency
We are right here in Texas and are able to help you shop multiple carriers-not just one.

Year-round Availability
We aren't just here when you enroll. We are available all year long to guide you with your insurance needs. That's the Texan way.

Personalized Help
Medicare is not a one-size-fits-all. Our first priority is the needs of our clients. We do a personalized consultation to help find the best plan options for YOU.
